The Untold Story of the World’s First Monkey Face Transplant
In the mid 1980s, a medical resident attempted a then-untested procedure

The profile of a baboon. (Photo: Jan-Nor Photography/shutterstock.com)
The world has now been witness to 30 human face transplants. The extent of these procedures has varied, and we have yet to see how the results will fare over time, but overall, they are seen as an increasingly viable option for those who have somehow lost their faces.
The first partial human face transplant was completed in France in 2005. But that operation didn’t materialize from nowhere: two decades before, a plastic surgeon named Thomas Loeb claims to have performed the first complete primate face transplant—on a monkey.
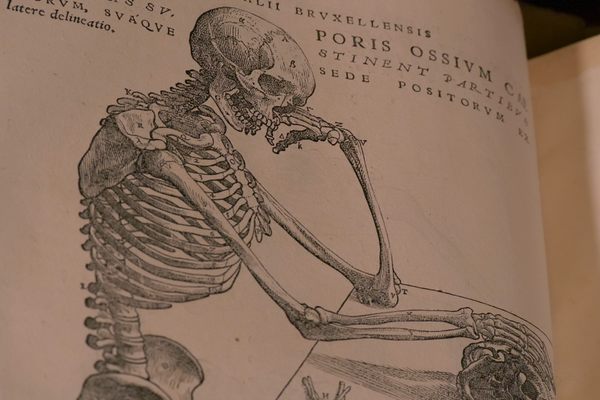
Dr. Loeb, then 32, was in his final two years as a resident at Baylor College of Medicine in Houston. The pioneering operation took about five hours, and Loeb went on to win the award for paper of the year at the Plastic Surgery Educational Foundation Senior Residents Conference in 1986. Though the experiment didn’t make it into the official scientific literature (Loeb presented it, but did not publish), it was one of the first of its kind, and one that very few people have ever heard about.
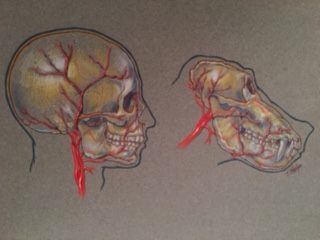
Human versus baboon vasculature. (Image: Thomas Loeb)
For Loeb, the transplant was a matter of demonstrating that the procedure was possible. At the time, he says, there really wasn’t anything near that. The ’80s was the age when microsurgery had just started, and Loeb had become skilled in the area. As a chief resident in general surgery, from 1983 to 1984, he had performed a number of head and neck cancer operations, familiarizing him with the anatomy.
“I came up with the idea sort of like lightning,” says Loeb. When he brought it up, his professor told him that there was nothing yet published about face transplants, that no one had ever done it, but that he’d always wanted to.
Loeb knew that the facial anatomy of humans and baboons is relatively similar, and believed that he understood how to perform the procedure anatomically—how to plug in the nerves, arteries, veins, and blood vessels. Baylor College has a very active animal lab with advanced equipment for animal monitoring, anesthesia, and euthanasia, and just a few hours away, in San Antonio, Texas, is a baboon colony, part of the Southwest National Primate Research Center.
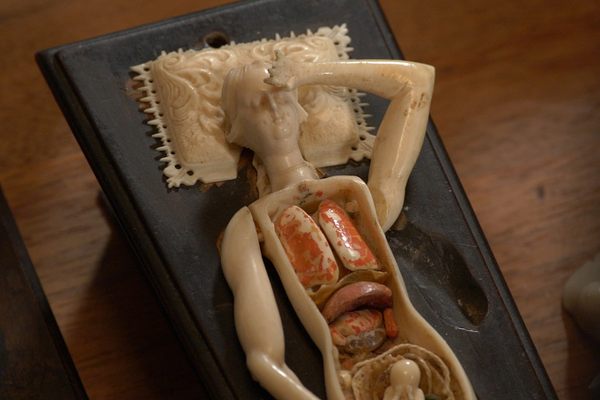
Loeb submitted a research proposal, which was met with support from his professor as well as $10,000 in research funding. The budget allowed him to acquire the cadavers of several of the colony’s baboons, who had died during a recent and unusual deep freeze. Loeb then completed a number of both baboon and human cadaver dissections, using dye studies in the arteries and veins to confirm that the proposed procedure would, in fact, be possible. He presented his research to the powers that be at Baylor, and they gave him the go-ahead to do a live transplant, under the condition that the animals would afterwards be euthanized, to prevent further suffering.
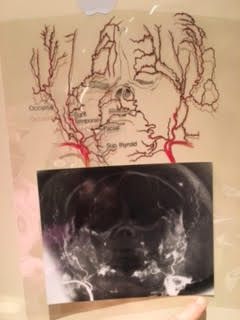
An angiogram of a human cadaver face and scalp as it would be transplanted. (Images: Thomas Loeb)
Loeb had two live baboons under anesthesia. The operation itself, he says, was exhausting. “I spent many, many hours taking the face off of both of them and transplanting to one of them,” he recalls. Once the transplant was complete, he did a fluorescein angiogram, a test that involved injecting fluorescent dye into the bloodstream to show that there was still functional blood supply and circulation. Though the best test would have been to see if the skin was still alive four days later, the procedure was still a success. “We were able to show that we could do it, and it could work,” Loeb says. “It was definitely a pioneering moment.”
Though his experiment generated a lot of excitement and interest, Loeb says he didn’t follow the field of face transplants very closely afterwards. He thought of his research as a really interesting thing, but there were a lot of fundamental issues and ethical questions involved. “I still think it’s a pretty impractical thing,” he says. “I find very rare instances in the world where I think it’s justified.” He mentions key issues like immunosuppression and inflexible scar tissue. “So my feeling was, Gee, what’s the point, what’s somebody gonna do this for? There’s tremendous risks towards health issues, cancer, heart problems—just to make a face that mostly works like a mask? If you got it to work like that.”

X-ray images of the right and left arm after a hand transplant operation in 2015, 16 years after the first successful hand transplant. (Photo: ‘Upper Extremity Composite Tissue Allotransplantation Imaging’/ CC BY-SA 4.0)
Early research on skin grafting goes back to Dr. Vilray Blair in 1910, while the first live organ transplant took place in 1954, performed on a kidney by surgeon Joseph Murray, earning him a Nobel Prize in 1990. The first successful hand transplant was completed in 1999.
While Loeb’s experiment was standard at the time, attitudes towards animal testing have continued to shift. Experiments on mice and rats attract less attention and are less expensive, meaning a lot less testing in big animals. However, animal tests continue to prove critical in providing a basis for human transplants; Chinese doctor Xiaoping Ren, for example, has recently worked with over 1,000 mice in his research on head transplants, and now wants to experiment with primates.
Interestingly, though Loeb appears to have performed the first monkey face transplant, in 1970, a man named Robert White performed the first monkey head transplant. More recently, an Italian surgeon named Sergio Canavaro has said that he will perform the first human head transplant (other doctors prefer to call it a body transplant) in December 2017, an announcement that has been met with skepticism and distrust. But is it possible that, like the face transplant, such a procedure will become normalized? The number of ethical discussions on face transplantation peaked in the years before and after the first instance in 2005, and then continually decreased.
What’s been happening since, says Loeb, has been interesting, and continues to change. “Operations are taking 20 hours or more with a lot of people doing them. They’re not taking the exact same plane as I did—probably less scar tissue and a little better function.” It’s an operation involving millions of dollars—but if that million dollars enables someone to walk to the corner store and not have everybody stare, then maybe that’s okay, says Loeb. Maybe, he adds, that in another 20 years it will be only $100,000, the technology getting better and better.

Face transplant recipient Jim Maki speaking to an audience at the Natick Soldier Systems Center in 2012, alongside Dr. Bohdan Pomahac. (Photo: US army staffman/Public Domain)
Dr. Maria Siemionow, who in 2008 performed the first near-total face transplant, says that she remembers encountering Loeb at a surgical conference, though she never saw his work in the scientific literature. Siemionow, author of The Know-How of Face Transplantation, says that her own preparation required 20 years of practice, working with a team of surgeons and other professionals on experimental animal models, cadaver studies, and the ethical and legal issues—a huge undertaking, she says. Siemionow mentions there have been other studies with monkeys doing partial, though not full-face transplantations.
Nowadays, however, she says that animals are used more to test anti-rejection therapies, the major obstacle right now being the need for life-long anti-rejection immunosuppressant medications, which have many side effects. Siemionow and other scientists, with multi-million dollar funding from the Department of Defense, are testing new therapies which would be safer and open up a much broader spectrum of patients.
From Loeb’s experiment in 1985 to the most recent and most extensive face transplant in 2015, the science has advanced quickly. Hopefully, in the future, we’ll get even better at saving faces.



















Follow us on Twitter to get the latest on the world's hidden wonders.
Like us on Facebook to get the latest on the world's hidden wonders.
Follow us on Twitter Like us on Facebook